Toxoplasmosis – September 2019

History
A 42 year old female presents with one week of blurred vision in the left eye. She states that a week ago she had a “spider bite” and subsequently developed flu-like symptoms. As a result, the patient was started on doxycycline but noticed the vision change the day after the symptoms started. She has no significant past medical history and was not on any medications except the doxycycline. Her vision in the right eye was 20/20-1 and in the left eye she was 20/30. IOP was 12 in both eyes. There was no APD and CVF were full, however she had a central scotoma on Amsler grid testing. Her anterior segment exam was normal.
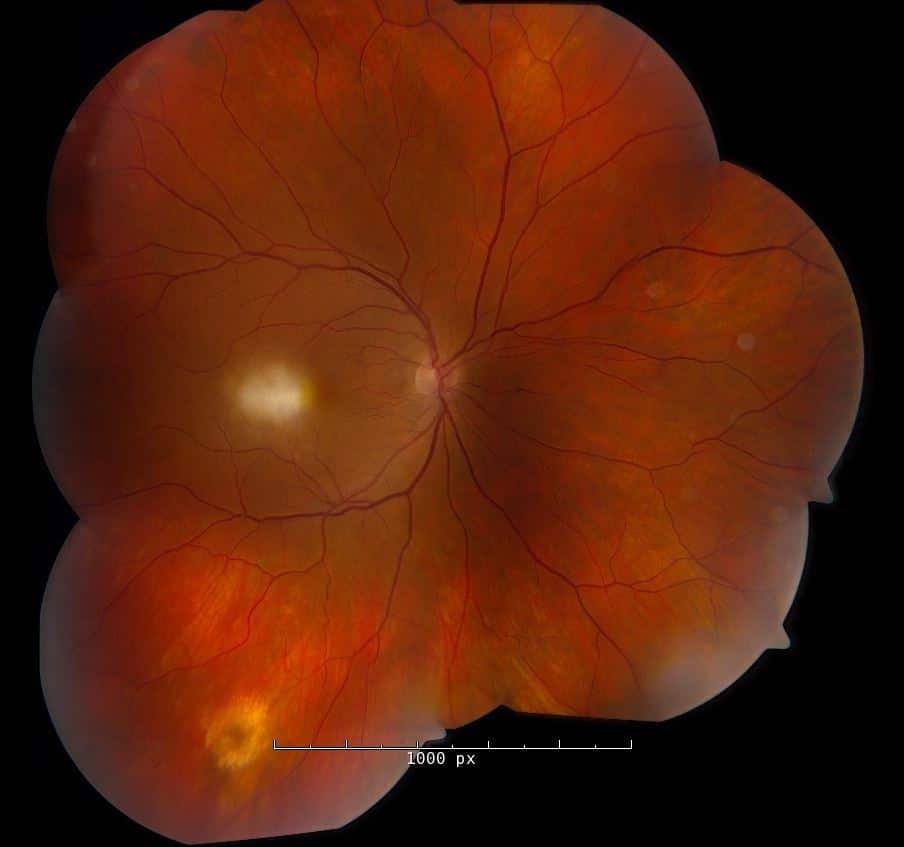
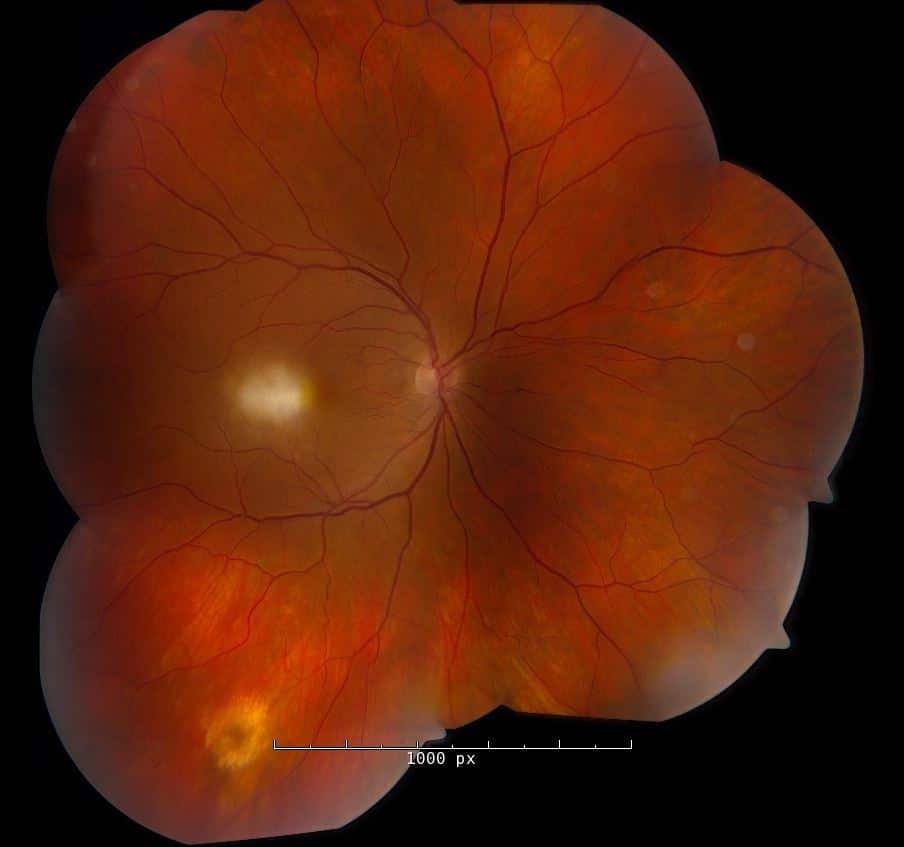
Evaluation of her posterior segment demonstrated clear vitreous OU. Below are her fundus photos:
Exam:
Vision was CF (count fingers) in his right eye and 20/25 in his left eye. IOP was 48 and 16 in the right and left eyes, respectively. Confrontation visual fields showed a central area of field loss OD, but periphery was intact otherwise. Anterior segment exam was significant for trace cell OD.
Evaluation of his posterior segment demonstrated rare vitreous cell OD. Below are her fundus photos:

Left fundus was unremarkable
Fluorescein Angiogram of the right eye (below) demonstrated leakage of the central macular lesion and staining of the inferior, peripheral lesion.

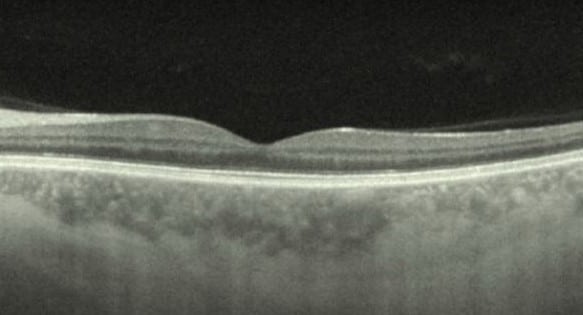
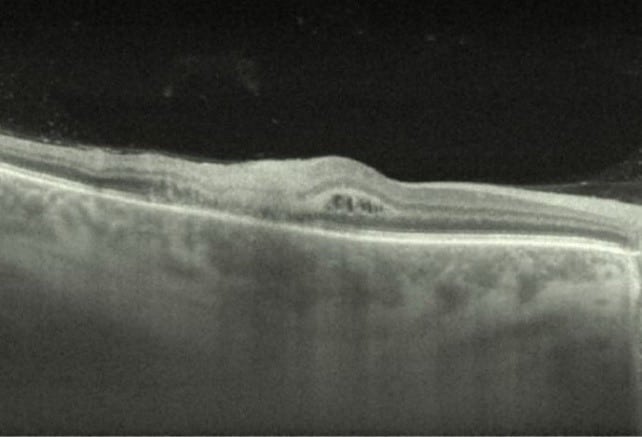
OCT: Left eye (top image) demonstrated normal foveal contour and no abnormality of the retinal layers or RPE; Right eye (bottom image) showed intraretinal distortion with loss of foveal contour and hyper reflective material in the outer layers.
Differential Diagnosis:
- Toxoplasmosis
- Syphilis
- Tuberculosis
- Sarcoidosis
- Viral Retinitis (CMV, HSV, VZV)
- Bartonella
Discussion:
Outer Retinal Toxoplasmosis Chorioretinitis
Toxoplasmosis is the most common infectious chorioretinitis in humans. The organism, Toxoplasma gondii, is found in a wide range of animals but the definitive hosts are cats. Rates of human infection are highest in tropical areas with most cases found in patients from locations such as Brazil and Africa.
Patients typically complain of floaters and blurred vision. The classic finding is described as a “headlight in the fog” demonstrating a white, focal retinitis with overlying vitreous inflammation. Often, there is a nearby pigmented retinochoroidal scar. Other common findings include keratic precipitates, inflammatory ocular hypertension, and retinal vasculitis. Diagnosis is mainly clinical, but the use of IgG titers is reassuring and can help rule-out disease. PCR of aqueous humor or vitreous fluid can be helpful in atypical cases.
Not all lesions require treatment, but in our patient, it was both macular threatening and he had significant visual impairment. Other indications include optic nerve lesions, large lesions, immunocompromised patients, or pregnant patients. Treatment involves “triple therapy” with a combination of systemic pyrimethamine, sulfadiazine, and corticosteroids. The addition of Bactrim, clindamycin, or azithromycin is also used in high risk lesions or atypical cases. The patient was started on triple therapy plus Bactrim as well as timolol for the elevated IOP and is scheduled for close follow-up.
References:
- Kim SJ, Scott IU, Brown GC, Brown MM, Ho AC, Ip MS, Recchia FM. Interventions for toxoplasma retinochoroiditis: a report by the American Academy of Ophthalmology. Ophthalmology. 2013 Feb;120(2):371-8. doi: 10.1016/j.ophtha.2012.07.061. Epub 2012 Oct 11. Review. PubMed PMID: 23062648
- Schachat et al; Ocular Toxoplasmosis, Chapter 88; Ryan’s Retina, 6th Ed.

